|
Gardening is a rewarding and relaxing hobby, but it can also be hard on your back. Long hours of bending, lifting, and kneeling can strain your muscles and joints, leading to pain and stiffness. To prevent back problems and enjoy your time in the garden, follow these simple tips:
1. Warm up before you start. Gardening can be a real workout, so warming up your muscles first is a good idea. Try a brisk five-minute walk and some stretching exercises. One relatively gentle stretch is the back-flexion exercise, in which you lie down on your back, then pull both knees to your chest while bringing your head forward. 2. Lift with support Lifting heavy pots, bushes, and full watering cans without proper back support can injure the discs, muscles, and/or ligaments in your back. To lift in an ergonomically supported manner, begin by squatting and not bending at your waist. Use both hands to hold the object, keeping it close to your body, and slowly straighten your legs as you stand. To minimise lifting, use a waggon, dolly, or other lifting aids to carry heavy items from place to place. Fill large watering cans just halfway and consider alternative watering options, such as soaker hoses or automated irrigation systems. 3. Take frequent breaks. It’s easy to lose track of time when you love being out in the yard. Take a water bottle with you as a reminder to take frequent breaks and hydrate yourself. If you’ve been in one position for a while, do some stretches during these breaks. Also, avoid doing the same kind of task, such as pruning, for a long period of time. Switch to another activity and rotate these tasks periodically. 4. Get support from kneelers and chairs. Getting down on the ground—and then standing back upright—can be painful or even impossible, depending on your level of pain and flexibility. Heavy-duty kneelers, especially those with raised, padded handles, can help you get up and down, allowing you to use your arm strength to aid in the process. Kneelers usually include a well-cushioned base to reduce stress and impact on your knees and back. Many kneelers also convert to low chairs. You can also use wearable or moveable knee pads for extra cushioning. 5. Use tools with long handles. Tools with long handles, such as forks and trowels, can help you reach the soil without bending too much. Some tools have extensions or telescopic arms, which reduce your need to stretch. Use pruners and loppers that have a ratchet system. This makes cutting easier and saves pressure on the back and shoulders. Keep the blades sharp to avoid extra strain. Put secateurs in a holster attached to your belt. This avoids having to constantly bend down to pick them up. By following these tips, you can keep your back healthy and enjoy gardening without pain.
0 Comments
4 Ways to Prevent an All-Too-Common Condition
When was the last time you or someone you know suffered an episode of back pain? Chances are it wasn't that long ago. It might have forced you to miss work, take painkillers, anti-inflammatories or other medication, or just deal with the pain longer than you wanted to. Wouldn't it be wonderful to do some simple things to try and prevent back pain from happening in the first place? Here are a few easy ones to get you started. In the new millennium, the health care pendulum has swung from treating symptoms toward prevention. It is a way of thinking that is analogous to going to the dentist for your six-month check-up or taking your car in for regularly scheduled maintenance - you avoid problems before they start, rather than waiting for something to happen and then "dealing with it." By that time, your car may be in the junkyard and you may be relegated to long-term medication or even surgery. Back pain is the perfect example of a symptom too many people treat instead of preventing, and the consequences are staggering. It is the most frequent cause of activity limitation in people younger than 45 years old. Approximately one-quarter of adults reported having low back pain lasting at least one whole day in the past three months and 7.6 percent reported at least one episode of severe acute low back pain within a one-year period. With all that said, how are you going to prevent back pain? Here are four things you can start doing today to reduce your risk of suffering back pain and its costly (physically, emotionally and financially) consequences: 1. Get Adjusted by Your Osteopath Your muscles, bones, and ligaments are stressed continuously by normal daily activities: driving, sitting at the computer, lifting your kids, doing exercise and countless other things. These little stresses add up over time and misalign the joints of your spine, arms and legs. The misalignments can then lead to muscle tightness, spasms, joint stiffness and pain. Although osteopaths commonly see patients who are in pain, getting spinal tune-ups when you are feeling "fine" will keep you feeling fine. Adjustments will put the bones and joints into healthier positions, which will also help muscle tone. Generally, if you get adjusted while you're in pain, it will take longer to heal, whereas if you get regular or maintenance adjustments, you can avoid terrible episodes of pain before they even start. That's because keeping the spinal and extremity joints in good alignment will help your nervous system and immune systems function at their best. Even when you think you are feeling good, osteopathy can make sure you stay that way. 2. Practice Proper Ergonomics Think safety: When you make your everyday activities safe to perform, it will help reduce the undue stress on your body. This includes having your computer work stations at home and at your office set up properly for your body. Generally speaking, the keyboard height should be the same height as when your arms are comfortably at your side with the elbows bent. The mouse should also be close to your dominant wrist while your arms are at your sides. Avoid poor posture: Whenever you sit, it is safest to sit on a full-back chair with plenty of support. Crossing the ankles is fine, but do not cross your legs. This puts tremendous pressure on the lower back, contributing to back pain. Also, if you are experiencing low back pain, it's a good idea not to sit on the couch or sofa, since they are typically too soft and unsupportive for the low back. Low Back Pain: One Symptom, Many Potential Causes (Including the Following) • Strenuous activity, overuse or improper use (repetitive or heavy lifting, vibration, pressure, etc.) • Physical trauma, injury or fracture • Obesity (often caused by increased weight on the spine and pressure on the discs) • Poor muscle tone in the core or stabilizing muscles of the back • Tightness, spasm, injury and strain of back muscles • Joint problems (e.g., spinal stenosis - narrowing of the spinal canal, which compresses the spinal cord and nerve roots) • Protruding or herniated (slipped) disk • Arthritis or degeneration of vertebrae due to stress and the effects of aging - osteoarthritis, spondylitis (inflammation of the spinal vertebrae), compression fractures, etc. Lift properly: When lifting items, use the legs and the trunk of the body rather than the arms. Always bring objects closer to your abdomen or chest, as that is the center of gravity and support for most people. Try to avoid bending the back while you lift. Sleep well: The most supportive position for the body during sleep is on your back with a pillow under your knees. The next best position is on your side with a pillow between your knees and your head on a pillow that is thick enough to span the distance of your neck to the shoulders. A neck pillow that is too thin will kink the neck and could lead to neck and upper back pain down the road. 3. Exercise Regularly We all know how important it is to participate in some type of regular exercise. Some of you already do that. Whether it be walking, playing sports or going to the gym, make sure you set up a program that keeps you consistent. Exercise helps the human body in so many ways, but one of the most important aspects involves stretching and strengthening your back muscles. Often these muscles are referred to as core muscles of the body because they are located very close to the spine. The core muscles help move and protect your spine when it is stressed or strained. By keeping them flexible and toned, you prevent pain and injuries from happening. When you are developing an exercise plan, talk to your doctor for ideas on what areas of the body you should specifically focus on to get maximum results, both in terms of overall fitness and protecting the back from injury. 4. Avoid Unhealthy Lifestyle Habits Stress. Emotional stress can cause muscle tension, which can lead to back pain (it also can lead to heart problems, chemical imbalances, an inability to sleep and a host of other bad things). It's always hard to maintain balance in your life between work, family and play, but it goes a long way toward helping your emotional stress. Reducing stress can be as simple as scheduling some quiet time to be alone, doing yoga or meditation, taking a bath or just sitting and doing breathing exercises. Whatever activity you find relaxing or energizing, take time to do it. Downtime allows you to unplug from the world and get grounded. It also allows your body to reset itself so you can deal with the next crisis or problem that's sure to arise. Poor nutrition. Watching what you eat is another important factor to consider, because excess weight literally "weighs you down," which can contribute to back pain. Quite simply, losing excess weight in a healthy manner will take the pressure off your lower back and reduce stress on the vertebrae. It is truly amazing that our society is now making an active transition from listening to symptoms or pain to preventative health care. Now is the time for you to be able to take a more active role in deciding how your future health will play out. Armed with the tips discussed above, you can make changes now that will help your back and your overall well-being for years to come. The power of health is in your hands. The Back Pain Epidemic Back pain has become an epidemic in our modern society - up to 85 percent of all people will experience back pain at some time in their life, and it is the fifth most common reason for all physician visits in the United States. According to the statistics, if you're in a room with three other people, one of you has suffered low back pain for an entire day or more in the previous three months and only one of you (if they're lucky) will avoid suffering back pain at some point in their lifetime. By Kevin Wong, DC All too often, people attribute neck pain to tension and take medication to hide the symptoms. Sound familiar?
Luckily there's a better way... A study published recently in the medical journal Spine revealed many people are often a little hazy on when and where their neck pain started. This study, sponsored by the World Health Organization (WHO), started about seven years ago. WHO started the Bone and Joint Decade and set up a task force with the job of reviewing all the research about neck and associated disorders. They reviewed 31,878 citations, 1,203 reviewed papers and four research projects - it makes me tired just thinking about it! Sure enough, most people don't remember when their neck issue started. Researchers concluded, "There is usually no single cause of neck pain." Unless you have had an injury to your neck like "whiplash" from an auto accident, neck pain usually sneaks up on you. The study notes neck pain is quite common, and the majority find their neck pain is stubborn and recurrent to some degree. The task force also came up with a new classification of neck pain. They suggested four grades of neck problems, no matter whether it comes from injury, arthritis or any other cause. To paraphrase: Grade I: Neck pain that doesn't interfere with living. Grade II: Neck pain that does significantly interfere with living. Grade III: Neck pain associated with a "pinched nerve," causing radiating pain, weakness or numbness in the arm. Grade IV: Neck pain associated with tumors, infections, fractures and other serious conditions. As you might guess, most neck discomfort is Grade I and II. There was also acknowledgement that "Cervical manipulation is a reasonable option for people with Grade I or II neck pain", something osteopaths do on a daily basis. Osteopaths "adjust" the joints, muscles and connective tissues of the body to improve motion by reducing restrictions and nerve irritation, thereby reducing discomfort and increasing recovery. So, how fast can a patient with neck pain expect to feel better with osteopathic care? By chance an issue of JMPT, British authors studied which neck symptoms might respond the quickest to hands-on treatment. Overall, considering all possible neck area complaints, about 70 percent of patients reported immediate favorable responses to manipulation. However, if patients complained about more specific things like headaches, shoulder or arm pain, reduced arm or neck movement, neck pain, or upper or middle back pain, the percentage of those who reported immediate improvement in pain rose to an incredible 95 percent! The popular humorist Nora Ephron wrote a book titled I Feel Bad About My Neck, in which she describes her thoughts about being a woman getting older. Well, hating your neck won't make it better, but chances are a trip to the osteopath will. Despite increasing public and professional awareness, revised pain-management guidelines and other signs of change, the numbing numbers still stand out: an estimated 130 deaths a day due to an opioid overdose.
Could a lasting solution be as simple as visiting a doctor of chiropractic or other conservative care provider first? You probably know the answer, but now research is proving it. Case in point: a new national study comparing first provider choice with early- and long-term opioid use in patients with low back pain. Published in BMJ Open, this study evaluated short- and long-term opioid use based on initial provider type seen: conservative care practitioner (chiropractor, acupuncturist or physical therapist) or primary care medical physician (PCP). Participants included 215,000-plus U.S. adults diagnosed with new-onset low back pain and "opioid naive." The study defined early opioid use as "an opioid fill within 30 days of the index visit" and long-term use as "an initial opioid fill within 60 days of the index date and either 120 or more days' supply of opioids over 12 months, or 90 days or more supply of opioids and 10 or more opioid prescriptions over 12 months." Researchers evaluated inpatient / outpatient claims from patient visits and pharmacy claims to correlate first provider type seen with opioid use, finding that LBP patients whose initial visit was with a DC were a staggering 90 percent less likely to use opioids early compared to patients who saw a PCP first. Significantly reduced odds for early opioid use were also noted for acupuncture and physical therapy patients. LBP patients who first visited a doctor of chiropractic or other conservative provider were also less likely to use opioids long term compared with patients visiting a PCP. ER physicians, orthopedic surgeons, neurosurgeons and rehab physicians were also included in the analysis. Patients visiting any of the above MD specialists first also had lower odds of early opioid use compared to primary care physicians (although not as significant as visiting a conservative-care provider), with the exception of ER physicians (dramatically higher odds for early use compared with PCPs). However, odds for long-term use were not significantly different compared to primary care providers for all of the above specialist types, with the exception of rehab physicians (still significantly lower odds compared to PCPs). If that's not enough proof, a second study, this one published in Pain Medicine, reviewed six previous studies involving more than 60,000 participants with spinal pain, finding that patients who saw a chiropractor were 64 percent less likely to use opioids compared to patients who visited another type of health care provider. It makes sense that patients who visit chiropractors are less likely to use opioids, since chiropractors provide nondrug, nonsurgical care. But the bottom line is, visit a chiropractor, reduce your risk of using a dangerous opioid! In light of the sobering statistics on opioid deaths, visiting a chiropractor for your pain could be a life-saving decision. Many people suffer from back pain and headaches, so if you're one of these people you're not alone. Chronic back pain and headaches are among the most common disorders worldwide and can significantly affect a person's life. Just as troubling, experiencing one of these conditions may raise your likelihood of experiencing the other.
There's also some good news, the fact that these issues may be connected means that one solution may help with resolving both disorders: Osteopathic care. According to a large scale research paper in the Journal of Headache and Pain, people who suffer from chronic back pain or chronic headaches are about twice as likely to suffer from both. The paper found 14 studies that reported an association between "primary headache disorders and persistent low back pain." Although the researchers do not find the cause of the connection between these two conditions, other studies have found links suggesting that dysfunction in the body, particularly involving the spinal joints and spinal nerves, can be a contributing factor with both headaches and back pain. That makes osteopathic care a great option when you're experiencing either condition – or both! Since an osteopath can help both back pain and tension headaches, there's a good chance that if you're only suffering from one, osteopathic care may prevent the other from occurring at all. Now that's a two-for-one win with osteopathy! Regardless of a doctor’s specialty, the school they graduated from or their years of experience, they can’t cure headaches, mend broken bones or heal a wound. Only you can do that… If your healing ability isn’t impaired.
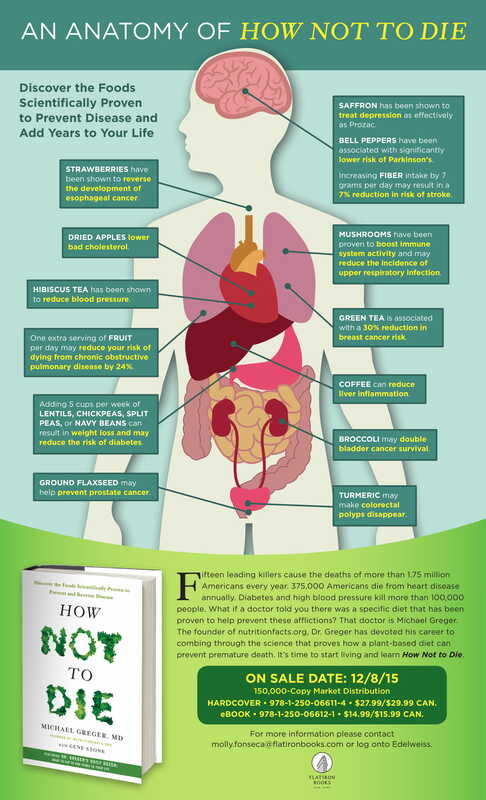
Your natural healing ability is responsible for the tremendous success that osteopathic patients enjoy. The only thing doctors can do, regardless of their discipline, is to help reduce barriers to the incredible healing ability you were born with. Which is why we’re interested in your skeletal and nervous systems. It’s what controls every movement, evey cell, tissue, organ and system of your whole body. The nerves along your spine are the most vulnerable part of your nervous system. By reducing any blockages to healing and nervous system compromise from the bones of your spine, you can then take over and do the healing! Do you know anyone whose healing ability needs a boost? Share this article with them.  Depression and anxiety are often unrecognised and as such, unaddressed in older adults. When these disorders are identified, a common treatment option, unfortunately, is the option that's become all-too-standard for any senior health issue: medication. But it doesn't have to be that way. Research suggests a simple mineral can help reduce depression and anxiety symptoms: magnesium. A study published in a peer-reviewed psychiatry journal found that among nearly 6,000 middle-aged and senior, community-dwelling adults, magnesium intake and depression scores; in other words, higher magnesium intake correlated with lower depression scores and vice versa. The findings remained significant even after adjusting for factors that might contribute to depression, such as socio-economic and lifestyle variables. Magnesium intake was assessed using comprehensive food-frequency questionnaires, a method that allows participants to chart their food consumption. Good sources of dietary magnesium include spinach, quinoa, nuts, black beans, avocado and dark chocolate. Magnesium supplementation is also an option if dietary sources prove insufficient. Talk to your doctor for more information. 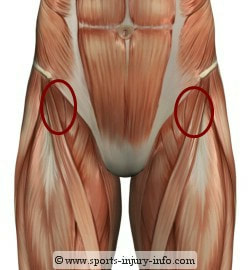 Site of common running injuries Site of common running injuries Leg pain pain is a common complaint, especially for people who run a lot. Although running is a great exercise it asks a lot of the muscles in the thigh and hip, and when we have been sedentary for a lot of the day sitting at desks this can be a lot for the body to cope with. A common area for people to experience pain is at the top of the thigh near the pelvis. It often goes with rest only to return as soon as we start training again. In order to understand what causes this problem we need to know little bit about the muscles around this area. The four main muscles in the thigh (Quadriceps) are mainly concerned with straightening the leg. One of the muscles also helps in assisting the hip flexors which bring the thigh to the front again so we can take the next step forward. However the main hip flexor is a little know muscle called psoas (it’s a silent ‘p’ if you want to impress your friends!). It attaches to the lower back and the inner thigh and can therefore cause problems in both these areas. If this muscle becomes chronically short, for example if we sit a lot, then it can’t operate at its full potential and struggles when we ask it to work hard when we’re running and sprinting. The reason for the pain at the top of the thigh is often not the psoas muscle itself as this is often working at below full potential, but the small muscle of the quadriceps I mentioned in the previous paragraph. As this assists in flexing the thigh it gets recruited when the psoas isn’t working correctly, and so becomes prone to injury and therefore pain and tenderness. We therefore experience thigh pain from the smaller accessory muscle at the top of the thigh, but it's not because this muscle isn’t working well, it's because it’s working too hard! To address the problem we need to treat the local inflammation but most importantly the shortened hip flexors. Just treating the injured muscle doesn’t address the root cause and so the injury keeps returning.  I am often asked what the difference is between osteopathy and physiotherapy, and which treatment would be most suitable. It can be hard to know who to see, and if one treatment is better for certain conditions. In today's private practice the two professions have many similarities and treat pretty much the same problems – equally successfully - albeit with a slightly different ideology and approach. Osteopaths view the body as a unique, interconnected system which has the ability to heal itself given the right environment. Osteopathic treatment focuses on correcting any disruption in this system - such as restricted joints, poor spinal alignment, muscle tension and imbalances and incorrect posture/movement patterns. Each person is assessed individually and not treated according to any set protocol. Osteopathic diagnosis and treatment is around 90% 'hands-on'. The techniques employed vary from soft tissue techniques such as massage and passive joint movements to joint manipulations (often referred to by patients as 'cracking'). They may also use ultrasound or acupuncture, and in many cases advise on lifestyle and posture. Exercises and/or stretches may also be given. Physiotherapists concentrate on restoring optimum function and performance to the problem area. As physiotherapy has been an intrinsic part the NHS for many years, the availability of funding has driven research and enabled studies leading to the development of 'treatment protocols' for the treatment of specific problems. Physiotherapy diagnosis and treatment is less 'hands-on' (around 60%) as more focus is given to observing movement and correcting technique. The techniques employed by physiotherapists vary from soft tissue techniques, such as massage and passive joint movements, to more extensive rehabilitation exercise programs. Ultrasound may also be employed. If people who primarily focus on muscles sit at one end of a spectrum (i.e. massage therapists to relax or personal trainers to strengthen) and people who primarily focus on joints sit at the other (i.e. chiropractors), physiotherapists and osteopaths sit together in the middle. So who should I see? It really comes down to personal preference. Both professions can successfully treat the same conditions, so if you still can’t decide my advice would be to ask around for a recommendation, as the individual is probably more important than the profession. But if you have a problem... Do something about it! It is more important that you see someone (physiotherapist or osteopath) rather than see no one at all!! |
AuthorJulian Newhill. Osteopath and Massage Therapist Archives
May 2023
Categories |
-
Horley
-
01293 369 442
-
[email protected]

 RSS Feed
RSS Feed